Alberta is home to world-leading research and advancements in cancer care thanks to the incredible work of our innovative research community.
By Fabian Mayer
Photographs by Jared Sych and Buddy Goodman
The steady advancement of cancer research is a success story decades in the making. The last 40 years have seen progress in every area of cancer diagnosis, screening, treatment and research. Today, Alberta leads the way for cutting-edge research, technological development and funding opportunities. Here, meet some of the innovators pushing for the next 40 years of breakthroughs.
Dr. Roy Park
Using PSMA PET to better detect prostate cancer

Prostate cancer is the most common cancer among Canadian men. An estimated 27,900 Canadian men were diagnosed with prostate cancer in 2024, accounting for 22 per cent of new cancer diagnoses in men. Sadly, about 5,000 Canadian men die from the disease annually.
But there is hope on the horizon. Advances in imaging technology promise to help doctors detect the disease earlier, diagnose more accurately and improve patient outcomes. Although still in the early stages of being adopted nationwide, Alberta is leading the way in implementing PSMA PET (prostate-specific membrane antigen positron emission tomography) imaging.
A constant challenge when it comes to accurately diagnosing prostate cancer is determining what stage it’s at, including if the cancer has spread. If cancer cells have spread beyond the prostate, to the bones, for example, surgery may be an unnecessary and ineffective treatment. Traditional imaging techniques, such as CT scans, are sometimes not detailed enough to determine the degree of spread.

Dr. Roy Park is the provincial senior medical director for diagnostic imaging at Acute Care Alberta, and he says PSMA PET imaging provides oncologists with a much clearer picture of a patient’s cancer.
“It’s the most cutting-edge examination you can do for prostate cancer, not only to stage it appropriately, but also to identify recurrence earlier,” Park says. “It not only means that you can avoid unnecessary surgery and that you can target therapy appropriately, but you can also catch it earlier and improve outcomes that way.”
Developed within the field of nuclear medicine, PSMA PET scans make use of radioactive tracer drugs. The radioactive substance is injected into a patient, where it binds specifically and exclusively to a part of prostate cancer cells, which are then made visible to a PET scanner.
“It really is the gold standard across the world, but it’s not yet widely used in Canada. So to be able to work with the Alberta Cancer Foundation and the Government of Alberta to be able to bring this test to Alberta, and to make it widely available here, is amazing and will really improve how prostate cancer is treated,” Park says.
Bringing the capacity for PSMA PET scans to the province has also opened pathways to new cutting-edge treatment methods for prostate cancer. The scans can determine eligibility for treatments requiring the same method of injecting a radioactive medicine that only attaches to cancer cells. Such treatments are currently available and can improve patient outcomes while also decreasing unwanted side effects.
Dr. Don Yee
Making radiation treatment possible for small cell lung cancer
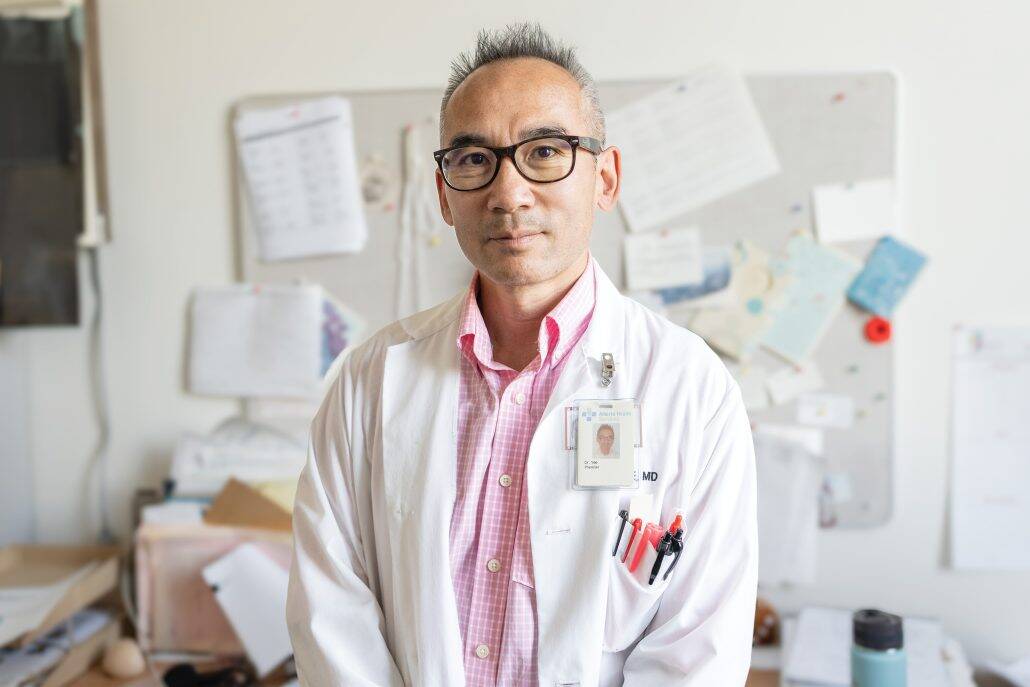
As an oncologist at the Cross Cancer Institute in Edmonton and the principal investigator of an ongoing clinical trial involving people diagnosed with lung cancer, Dr. Don Yee is at the forefront of improving treatment and outcomes for individuals with lung cancer in Alberta and beyond. His research focuses on a difficult-to-treat type of lung cancer known as small cell lung cancer. The cancer is hard to treat effectively because by the time it is found, it has often grown to quite a large size. Add to that, its location in the chest makes it almost impossible to safely deliver the radiation needed to effectively treat the disease.
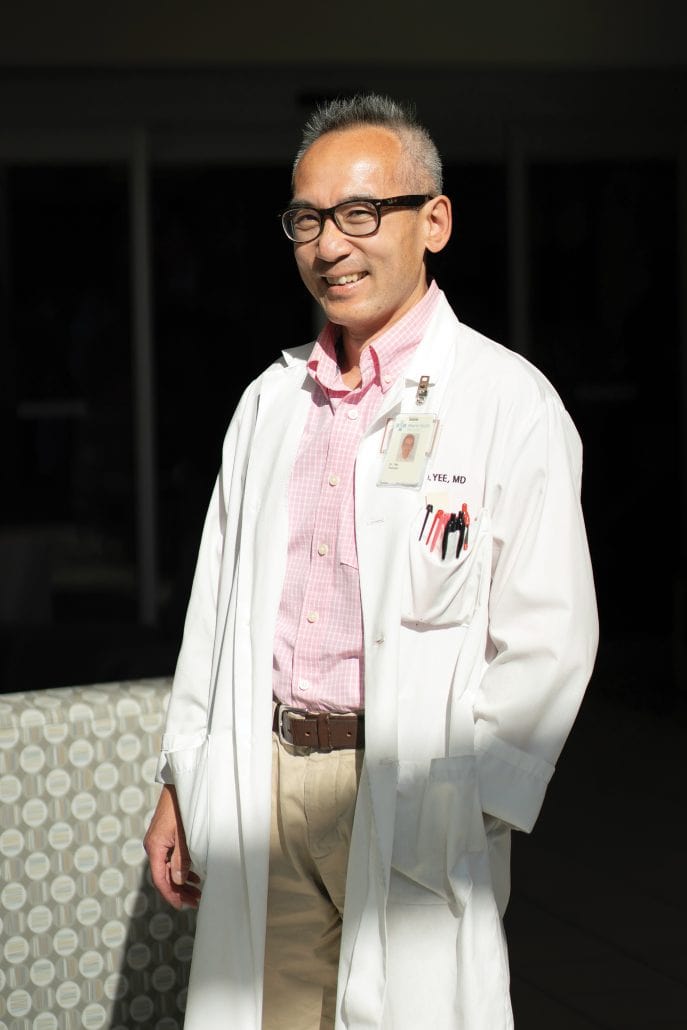
Yee is working to change that. Known as adaptive radiation, the approach Yee and his fellow researchers are using in their clinical trial tracks the size and shape of the tumour in real time over the course of radiation treatments. As the tumour changes shape or shrinks, the radiation dose is adjusted to match, thereby ensuring the tumour is targeted precisely and healthy tissue is avoided.
“If the trial is successful, we will define a way to safely deliver chest radiation for a wider group of patients with this type of cancer,” Yee says. “By doing that, you’re potentially offering patients with this type of lung cancer a chance of being cured, and if not cured, it could give them a chance of at least controlling their cancer for a longer period of time.”
Though not the most common, small cell lung cancer is one of the deadliest. This is in large part due to the difficulty of administering radiation treatment. The trial could harness ever-improving radiation technology in hopes of giving people with small cell lung cancer more treatment options and improving their outcomes.
“It used to be that past a certain size of tumour, we would just say there’s no way to give radiation to this patient. That patient loses all the benefits that they could derive from radiation therapy,” Yee explains. “It’s potentially a stepping stone to establishing a new accepted standard of care for giving radiation for this type of lung cancer.”
Dr. Steven Yip
Allowing for more targeted treatment with precision oncology

As an indication of just how far science and medicine have come, some of the most exciting areas of advancement in cancer treatment and research today didn’t even exist 40 years ago. Precision oncology is one such area of research. The relatively new field seeks to better understand specific tumour types, allowing for more tailored and effective treatment.
Scientific and technological advances enable researchers to delve into the genetics of specific cancer types in a highly detailed way. This allows for ever more precise differentiation of tumours into types and subtypes while simultaneously discovering where and how these tumours could be vulnerable. Dr. Steven Yip is a medical oncologist at the Arthur J.E. Child Comprehensive Cancer Centre in Calgary and the medical lead for Precision Oncology & Experimental Therapeutics (POET).
“Precision medicine is making a big impact in the care of patients with advanced cancers and unmet clinical needs,” Yip says. “We’re aiming to incorporate novel biomarkers and diagnostics into practical, clinically driven precision oncology research initiatives to impact patient care with cutting-edge medicines, tests and treatments.”

One precision oncology initiative being spearheaded by Yip, along with Dr. Omar Khan and Dr. Sasha Lupichuk, is the Alberta metastatic breast cancer registry. Through genomic sequencing of biopsies and surgically removed tumours, the project aims to create a comprehensive, province-wide database of breast cancer information. Yip hopes this approach will yield clues as to what treatments could be most effective for individual patients in Alberta.
“Some directed treatments target specific biomarkers. By identifying these patients earlier, we can offer this specific DNA testing or genomic testing, which can be performed on the tumour, either through a biopsy or when the tumour is removed at surgery,” Yip says. “Then we can look for individual genes and molecular signatures, which may tell us how their disease might behave. It could inform us how we should treat these individuals and could result in a more tailored and targeted approach for these patients.”
The ability to sequence the genes of cancer cells — something that was unthinkable just a few decades ago — has since become an extremely promising new area of research and cancer care.
Where hope meets healing.
On March 9, 2025, the official dedication of the Gay Young Systemic Therapy Unit at the Cross Cancer Institute in Edmonton took place, demonstrating the continued impact of the Alberta Cancer Foundation’s We Cross Cancer campaign.
Brought to life by the generosity of Gay Young’s friends and family, the unit stands as a living testament to the hope, care and compassion that Young so warmly shared with others. Quiet and spacious with bright windows and a nature-filled view, the unit has become an inviting and refreshing space for up to 40 patients to receive treatment every day. Efficiency and delivery of care were also considered in the design as the treatment beds and chairs are configured to make it easier for medical staff to support patients.
The Gay Young Systemic Therapy Unit demonstrates how innovative cancer research can be realized into life-saving treatments. More than 50 per cent of patients facing cancer will require systemic therapy as part of their treatment. Systemic therapies include chemotherapy, targeted therapy, hormone therapy and immunotherapy. These treatments circulate throughout the body to target cancer cells wherever they may be, making them especially important for cancers that have spread or are at risk of spreading.
Every year, more than 2,500 Albertans will receive treatment in this vital space, thanks to the incredible researchers, health care professionals and donors who make places like the Gay Young Systemic Therapy Unit possible.


